|
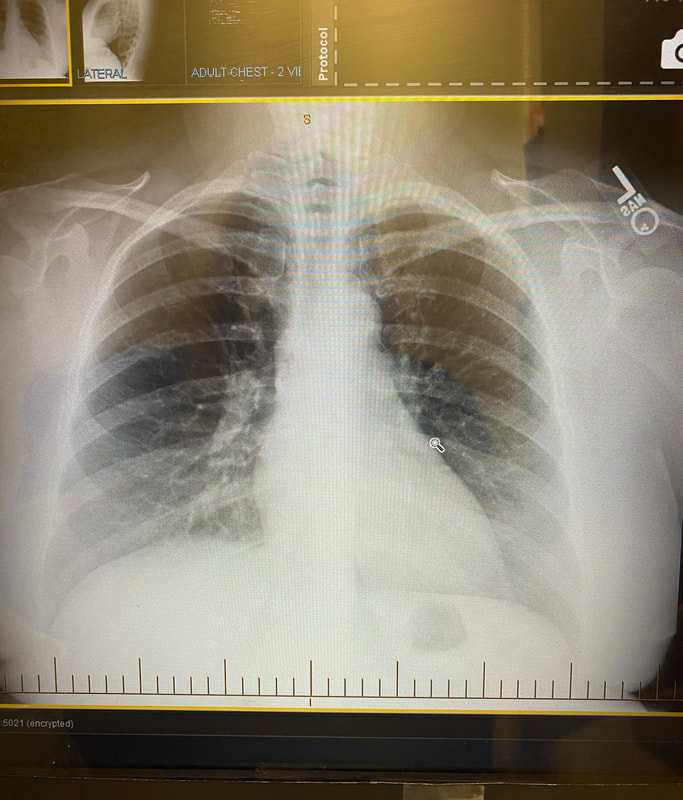
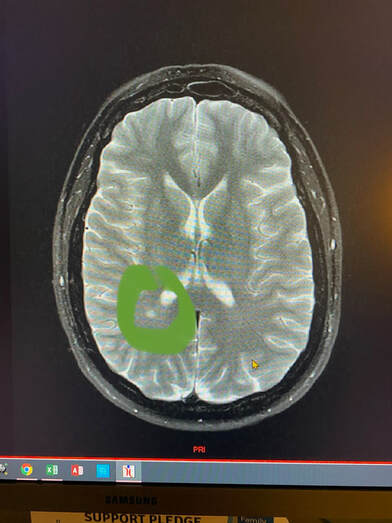
In 2016, at the age of 40, I received a sarcoidosis diagnosis that rocked my entire world. My kids were 4, 6, and 14 at the time. I was at the pinnacle of my NP career, and I was coming off a 2 year "break" from full-time work. From 2014-2016 I was working 2 or 3 days a week and was able to spend more time with my family. I was also able to go to the gym regularly and prepare healthy meals. I felt like my health was also better than it had been in the past 7 years. My sarcoidosis symptoms started abruptly in September and were very noticeable. I would walk to my car that was parked on a hill after work and be extremely short of breath (think huffing and puffing as if I had just sprinted 100 yards). I would go to the gym and feel completely wiped out after 20 minutes of my workout when normally my full hour workout left me energized and not depleted. I would walk out of an exam room and forget the name of a medication or stop mid-sentence when trying to give my nurse a verbal order. I also felt very dizzy and lightheaded and was not sure what was causing all of my symptoms. I decided to go see my colleagues in cardiology once I realized my blood pressure was dropping. My blood pressure was dropping as low as 80s/50s. I was also having numbness and tingling in both arms and hands and my hands were turning blue. I thought there had to be some type of blockage or blood flow issue. Ultrasound evaluation of my carotid arteries and upper extremities were normal. EKG, basic labs, and chest x-ray were normal. My echocardiogram (heart ultrasound) was the first test that came back abnormal. It showed an elevated pressure reading between my heart and lungs (pulmonary hypertension). My providers were not really sure what would be causing that because I was "so healthy." I plugged along from early September to late September before seeking a second opinion. My symptoms were progressing and persistent, and I knew something was not right with my body. My fatigue was worsening to the point I would count down the hours until I could get into bed. My shortness of breath was limiting my daily activities and I was beginning to cough every time I ate or talked for more than a few minutes. I also had an episode while driving where the left side of my face went numb and my breathing became very shallow and irregular. That sent me straight to my second opinion! That second provider ordered a chest CT and a brain MRI which were performed on a Thursday morning. That following Monday in early October, I was at work for a 12-hour day. I received a phone call mid-morning from a nurse in my second opinion provider's office. The nurse said "you have brain lesions and you need to see a neurologist to rule out MS (multiple sclerosis). You also have enlarged lymph nodes throughout your chest and you need to see an oncologist to rule out lymphoma." As you can imagine, I was in shock and called my manager to tell her I needed to leave for the day and to go speak to my husband and my parents. Did I mention my youngest child was 4 years old? Fast forward to a bronchoscopy mid-October with lymph node and lung needle biopsy as well as a trip to a neurologist which resulted in EEG and extensive lab testing. My neurologist ordered more MRIs and tried to ease my fears of MS (though he could not totally rule MS out). My pulmonologist was unable to get a conclusive diagnosis from the bronchoscopy and recommended a mediastinoscopy which would involve drilling through my sternum (breastbone) to remove lymph node tissue for biopsy. I told him that I felt a large lymph node above my left clavicle and we opted to have that node excised for pathology instead of the mediastinoscopy. That left supraclavicular node excision was done the last week in November under general anesthesia at the hospital since it was so close to my carotid artery and jugular vein. That node biopsy was negative for lymphoma and positive for non-caseating granulomas (the definitive diagnosis for sarcoidosis). I was started on 60 mg of Prednisone per day that would be tapered over 6-12 months and referred to a rheumatologist.
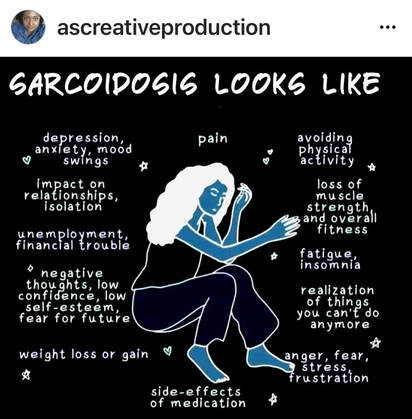
After starting high dose Prednisone in December of 2016, I was placed on weekly Methotrexate injections which (who knew at the time?) would last another 4 years. The only reason I stopped Methotrexate is because I later developed psoriasis (for that story, click here). I was finally able to wean off prednisone late May 2017 though the side effects lingered at least another 6 months. I plan to write an entire post on surviving long-term prednisone, but I will leave it at that for now. 2017 seemed somewhat stable throughout the end of that year, but the next 3-4 years had their own hiccups. Over those next 3-4 years I found out that the sarcoidosis was affecting my esophagus. 3 EGDs in 6 months and tons of other GI testing led to the conclusion that my esophagus has no peristalsis ("squeeze'). The only thing helping my food reach my stomach is gravity. This makes eating challenging, especially talking while eating (cough, choke). I also found out I had sarcoidosis spleen lesions, ocular involvement, and another fun lung condition called bronchiectasis. For the esophageal involvement, I take 2 pills per day for life. For the bronchiectasis, I take one pill twice a day for life. See how I organize my meds here. I have also been tested and monitored for small fiber neuropathy. The MS surveillance continues. My neuropathy is currently of unknown etiology, but my neurologist does think sarcoid plays a role. I was also sent to endocrinology at one point to check for adrenal insufficiency after steroids since my blood sugar and blood pressure still bottom out at times. Another hiccup involved an overnight hospital stay and a kidney biopsy (ouch by the way) after I noticed my urine was foamy like dishwashing liquid (that is abnormal and a sign of protein in your urine- tell your provider if you ever see this). I'm on another daily pill to help protect my kidneys for that confirmed renal sarcoidosis. Every year I see a rheumatologist, general cardiologist, pulmonary hypertension cardiologist, pulmonologist, gastroenterologist, neurologist, ophthalmologist, dermatologist, nephrologist, and my PCP and Gyn. I now see a counselor regularly to help me process all that I juggle. I have mandatory quarterly labs, an annual heart ultrasound, CT's and MRI's every year, breathing tests every year, and whatever else comes up. Gone are the days of a routine wellness visit or not meeting my deductible. Gone are the days of only taking a multivitamin. I sleep with oxygen mainly for the pulmonary hypertension, and I'm okay with that. It was my little secret until now. Right now, my sarcoidosis seems fairly well-controlled with Humira. When I met my rheumatologist in 2016, he told me he hoped he could get me into remission within 2 years. That was 5 and a half years ago. I haven't given up hope and I will continue to fight this fight as long as I can.💜 Below, I have included two great visual aids to raise awareness for our family and friends. The mental health effects of sarcoidosis are widespread and often overlooked by our clinicians. Sometimes just "being there" is all we need from our loved ones. 💜
I hope this post has raised your awareness of sarcoidosis whether you are a patient, loved one, or healthcare professional. As I told a friend after she learned of my chronic illness, "My entire life changed after being diagnosed with sarcoidosis, but I didn't stop living." I hope this offers hope to anyone who is newly diagnosed or any sarcoidosis patient struggling right now. I see you. 💜
4 Comments
Mary Estes
4/6/2022 05:52:54 pm
As I have said before, you are one special person and you mean so much to so many people. Just keep up the fight and hopefully you will be able to be blessed with a relief from this terrible thing you are living with.
Reply
amy cobb
4/7/2022 07:02:35 am
Thank you Mary! Your prayers and words mean so much to me!
Reply
Betsy Wertz Curley
4/7/2022 05:59:44 am
Thank you for telling your story. Mine is similar. I was diagnosed by a lung biopsy done in 2015. My diagnosis was Pulmonary Sarcoidosis. I also have had Fibromyalgia for 26 years. My biggest problem is extreme pain & fatigue. Since Covid, I am mostly house bound and only see close family and my Specialists. Including a Pulmonologist, Cardiologist and Nephrologist. I lost my career, which was a Real Estate Broker. I loved my career and it was a big loss to me. Not being able to concentrate was a big issue toward my retirement.
Reply
amy cobb
4/7/2022 07:04:17 am
Thank you for reading Betsy. My prayer for you is that you can begin to leave the house again (and feel good enough to do so). You are NOT alone and I see you, my sarcoidosis sister.💜
Reply
Leave a Reply. |